Diabetes: The History of a Public Health Crisis
By Tom PorterAround thirty million Americans suffer from diabetes, more than seven million of them undiagnosed, according to the Centers for Disease Control and Prevention. The number has grown markedly in recent decades—a threefold increase in twenty years, for example— and is predicted to keep growing. It’s a situation that Associate Professor of History and Environmental Studies Matthew Klingle finds concerning on a number of levels.

His current book project, Sweet Blood: Diabetes and the Nature of Modern Health, under contract with Yale University Press, explores how today’s health crisis grows from our changing relationships with nature and shifting patterns of social inequality in the United States and the world from the late-nineteenth century to the present day.
“How did diabetes go from a disease of largely affluence a century and a half ago—something we blamed on overeating and inactivity—to a disease today that’s associated with low socio-economic status?” Klingle asked. Furthermore, he explained, diabetes is increasingly seen as a disease that’s not solely caused by dietary choices, but other factors people often can’t fully control, like poor nutritional options and exposure to certain chemicals.
What is diabetes?
There are two main types of diabetes, both of them characterized by high blood sugar levels. The most common—affecting 90 to 95 percent of sufferers—is known as type 2 diabetes. It’s a condition where the body fails to produce enough insulin (a hormone made by the pancreas that regulates our intake of sugar) or to use insulin properly. It’s linked to poor diet, obesity, and lack of exercise. “A certain type of lifestyle can overtax the pancreas,” said Klingle, “as it works to produce the insulin required to metabolize all that food you eat and sustain those fat cells as you get larger.”
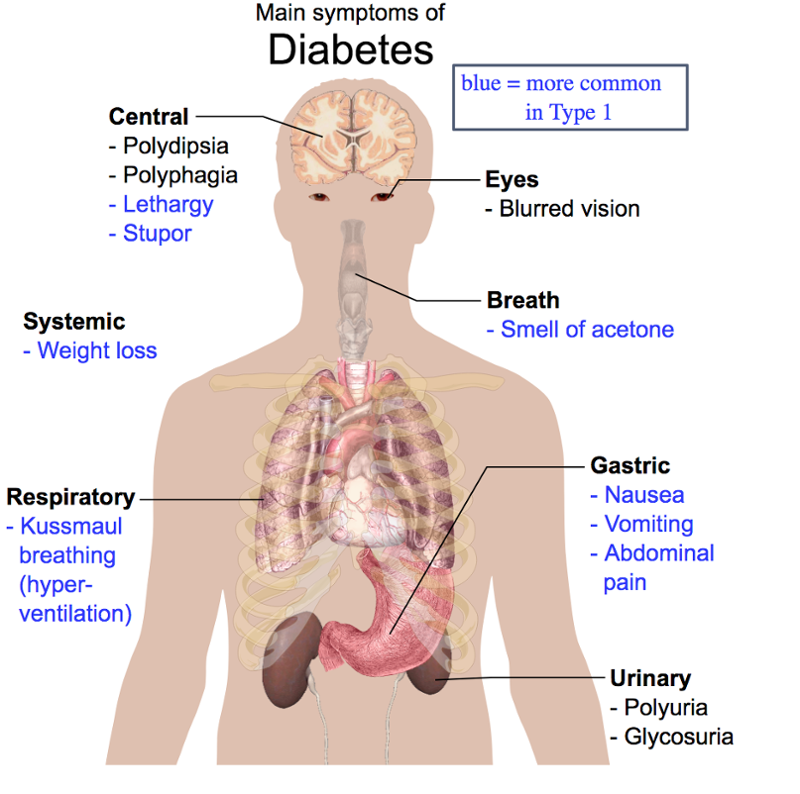
Type 1 diabetes is due to the loss of beta cells in the pancreas, which as a result fails to produce enough insulin to regulate blood sugar levels. The cause is unknown, although some researchers suspect possible environmental causes. A third variety of the disease, gestational diabetes, affects women during their pregnancy. Diabetes can lead to a range of serious and sometimes fatal afflictions, including heart disease, strokes, kidney failure, blindness, and loss of limbs. In 2015, it was listed as the seventh-leading cause of death in the US.
Why are poor people more at risk?
Diet and access to healthcare are supremely important factors when it comes to someone’s likelihood of getting diabetes, said Klingle, and they are invariably linked to a person’s socioeconomic status. Consequently, certain racial or ethnic groups are more prone to diabetes, he explained, as are people of lower economic means. According to the CDC, as of 2017, Native Americans had the highest prevalence of diagnosed diabetes, at around 15 percent, with African Americans and Hispanics at around 13 percent. Meanwhile, around 7 percent of America’s white population suffers from diabetes, with percentages increasing to above 12 percent for those individuals with less than a high school education.

“Many health researchers in the US have observed that the most important numbers for predicting your state of health are your zip code. This tells us whether you live near a source of pollution, for example, and whether you’re near a supermarket that sells fresh, affordable food, or in a so-called ‘food desert,’ where only convenience store-type food of poor nutritional quality is available,” said Klingle.
Access to affordable healthcare is also key. “Type 2 diabetes is largely preventable,” said Klingle, “and, if you have a regular healthcare provider, your physician should be able to tell you if you’re at risk, or if you’re what’s called ‘pre-diabetic,’ meaning your blood sugar is elevated but you’re not yet diabetic.”
“Many health researchers in the US have observed that the most important numbers for predicting your state of health are your zip code."
Endocrine disrupting chemicals
Not everything comes down to diet and lifestyle, however. The biggest chemical culprit when it comes to diabetes, said Klingle, is a group of substances called endocrine-disrupting chemicals, or EDCs. “Over the last few decades, a whole host of industrial chemicals known as EDCs have been identified that either mimic or block the role of hormones in our bodies. So, in the case of insulin, they prevent it from doing its job of processing glucose in the blood.”
Research suggests that these man-made chemicals have made their way into the environment and into the food supply, said Klingle, often passing into the fetus during development because the mother has ingested them. “EDCs may not be the sole reason for the spike in type 2 diabetes, but they could be a contributing factor, which, when added to the usual factors like obesity, could act as a tipping point in causing the disease.”
There are socioeconomic considerations at play here too, explained Klingle. “Exposure to these chemicals is very often linked to communities that are near places where they are disposed of, legally or illegally. In the same way that someone who is better off can afford fresh healthy food, they’re also less likely to be living downwind or downstream from pollution sources .”

What can be done?
The concern Klingle has is that, despite a growing body of research linking EDCs to health problems like diabetes, there is still no widespread acceptance among health professionals or government agencies. “Which is why our best hope lies in consumer action to pressure regulators into acknowledging these threats to public health.”
He cited the example of bisphenol A (BPA), an industrial chemical found in many packaging products, including baby bottles. Mounting concern over BPA leaking into the food chain, and the possible harmful effects of that, led to a high-profile consumer campaign. Many manufacturers subsequently agreed to offer BPA-free containers, and in 2012 and 2013 the Food and Drug Administration banned the use of BPA in baby bottles and infant formula packaging. However, the FDA still permits BPA in certain beverage containers and many food and beverage can liners.
Industry and regulators currently operate under a system that presumes chemicals are safe until proven otherwise, said Klingle, and that’s a problem. “There’s currently a backlog of tens of thousands of chemicals that have not been evaluated by federal agencies but are permitted onto the market because of our regulatory system. Some of these chemicals are likely benign,” he added, “but, for those that might not be, we may not know the effects on human health for many years.
“We should be more open to the so-called precautionary principle,” argued Klingle, “where chemicals must be proven safe before they can enter the marketplace.” In the meantime, he concluded, more healthy food options, not to mention regular health screenings, need to be made available if the US is to curb its diabetes epidemic.